

Author: Dr. Stephanie Wolstenholme, VMD
Melvin, a 4.5 yo MC Basset hound, was initially presented to the PASE Emergency Service on 2/19 for a 4 day history of coughing and tachypnea which was noted that day. He also vomited a few times during that 4 day time period, one of which contained a piece of ketchup packet.
On presentation Melvin’s temperature was 102.2 ℉, heart rate was 120 bpm and respiratory rate was 60 brpm. He had a mild increase in his respiratory effort and harsh lung sounds bilaterally. Diagnostics were declined by the owner and he was given a Cerenia injection and discharged with Clavamox for presumptive aspiration pneumonia.

Melvin returned the following day for lack of improvement, ptyalism and more significant coughing. He had received two doses of Clavamox. On re-presentation his temperature was 101.6 ℉, was slightly tachycardic at 156 bpm at rest and his respiratory rate was 60 brpm again with a slight increase in his respiratory effort. Harsh lung sounds were again noted.
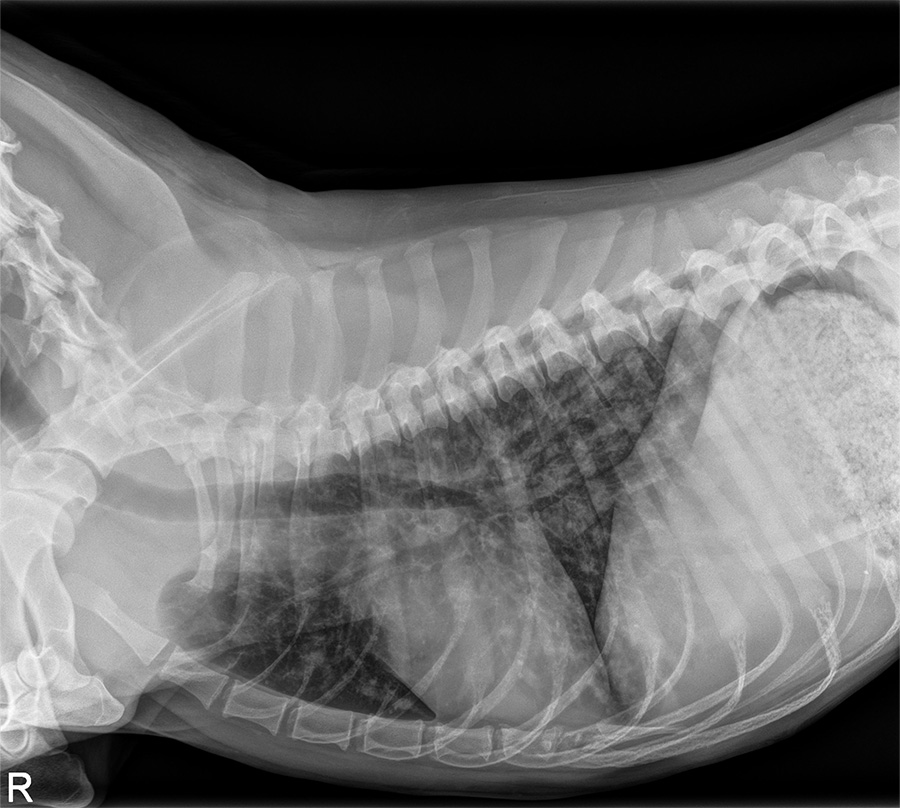
At this time the owner consented to performing diagnostics. Bloodwork was performed which revealed a marked eopsinophilia of 5.92 k/uL, a basophilia of 0.45 K/uL and a thrombocytopenia of 71 k/uL. An in-house blood smear confirmed the eosinophilia as well as a large number of neutrophils; the thrombocytopenia was suspected to be artificially low due to the presence of small and large platelet clumps. Thoracic radiographs were performed which showed: “Significant airway infiltrates are identified throughout the lung. In the periphery of the lung on the lateral projections superimposed over the heart and diaphragm, the airways appear to fill with fluid density likely indicating mucous plugging. The cardiac silhouette and pulmonary vasculature appear normal. There is evidence of severe airway inflammation. There was no mention of smoke or noxious agent inhalation, which raises concern for either viral or parasitic causes.”
Melvin was admitted to the hospital and a SNAP 4Dx was performed which was negative x4. A respiratory PCR panel was submitted to Cornell (and subsequently returned negative). A Baermann fecal analysis was submitted to PennVet. While diagnostics were pending Melvin was hospitalized in oxygen and was receiving empiric deworming with Panacur for possible lungworm or other parasitic disease given his eosinophilia, theophylline and continued Clavamox. After 24 hours of hospitalization there was no improvement in his respiratory signs so he was also started on prednisone at 1 mg/kg/d for suspected eosinophilic bronchopneumopathy. This improved his signs and he was discharged after 48 hours in the hospital.
2 days after discharge the results of the Baermann were returned which was positive for Crenosoma vulpis, or fox lungworm.
Crenosoma vulpis, a parasitic nematode primarily affecting foxes, has increasingly been identified in domestic dogs, especially in areas where wildlife populations overlap with urban environments. Although Crenosoma vulpis is more commonly found in wild canids, it is gaining significance as a cause of respiratory distress and disease in domestic dogs.
The lifecycle of the parasite involves a definitive host, such as a fox or dog, and an intermediate host, usually a gastropod like a snail or slug. The infection process begins when a dog ingests a contaminated gastropod containing third-stage larvae (L3). Once ingested, the larvae migrate through the dog’s digestive system, reaching the lungs where they mature into adult worms. Infected dogs release larvae in their feces, which are then consumed by intermediate hosts, continuing the cycle.
The clinical signs of Crenosoma vulpis in dogs are often related to respiratory distress, as the adult worms reside in the bronchial tree and lungs. Common symptoms include: cough, tachypnea, dyspnea, exercise intolerance, nasal discharge, hemoptysis and/or pneumonia. Diagnosis of fox lungworm requires a combination of clinical suspicion, history, and laboratory tests such as:
- Fecal exam: gold standard is identification of L1 larvae in a dog’s feces, however these larvae can be difficult to capture due to their small size and low fecal shedding rates
- Baermann fecal analysis
- Bronchoalveolar lavage: to collect fluid from the lungs for cytology, culture and sensitivity and sometimes this can also contain larvae or adult worms
- Imaging such as radiographs, CT scan or bronchoscopy
Treatment of Crenosoma vulpis in dogs typically involves the administration of anthelmintic drugs, which target the adult worms and larvae, and typically includes fenbendazole, ivermectin or milbemycin oxime. Antibiotics can also be useful to treat secondary infections and steroids and/or bronchodilators may also help to treat secondary airway inflammation.
Following the results of the Baermann Clavamox was discontinued. Melvin had received an initial 3 day course of Panacur but when the positive results were returned he was started on another 14-day course as lungworm requires a longer treatment course than standard GI parasite treatment. His steroids were tapered off over 2 weeks to treat any inflammation secondary to worm die off and his theophylline was continued for a few additional days and then stopped.
We are happy to report that Melvin responded well to his treatments and has made a full recovery! We hope he avoids any slugs/snails in the future!

