

Author: Katie Zatroch DVM, DACVAA
If you’ve ever wondered whether sacrococcygeal epidural blocks are worth adding to your anesthetic toolbox, the answer is…yes! This simple, minimal-risk technique provides targeted perineal analgesia without motor block to the pelvic limbs. In cats especially, it can make challenging procedures like urethral obstruction catheterization far smoother and less stressful, for both the patient and the clinician.
Much like any epidural or peripheral nerve block technique, the goal of the sacrococcygeal epidural is to enhance the analgesic profile of the drug protocol and reduce the systemic sedative/anesthetic requirements of the patient. The frequent feedback received following the incorporation of this technique is the stability of the sedation/anesthesia and a reduction in the use of rescue medications during the procedure.
Relevant Anatomy
While performing any locoregional block, it is first essential to understand the anatomical space and best orient yourself.
Extending caudally, dogs and cats have 7 cervical, 13 thoracic, 7 lumbar, 3 sacral and approximately 20 coccygeal (tail or more properly termed “caudal”) vertebrae. The sacral vertebrae are fused into a single entity called the sacrum. During this epidural, our goal is to enter the sacrococcygeal space between the sacrum and the first coccygeal vertebrae, or the intercoccygeal space between the first two coccygeal vertebrae.
When approaching these spaces, it is helpful to understand the layers of tissue that will be encountered. From dorsal to ventral, expect that your needle will encounter the skin, subcutaneous tissue, the supraspinous ligament, the interspinous ligament, and the ligamentum flavum (“yellow ligament”) before entering the epidural space.
Throughout most of the length of the spinal canal, the epidural space lies dorsal (above) to the intrathecal or subarachnoid space, which contains the cerebrospinal fluid that bathes the spinal cord. Caudally, the spinal cord tapers into a conical structure called the conus medullaris. In large breed dogs, the conus medullaris extends only as far caudal as the 6th or 7th lumbar vertebrae, and in small breed dogs and cats it can extend as far caudally to the lumbosacral space. The only instance in which the conus medullaris may extend as far caudally as the sacrum is in neonatal dogs and cats. The subarachnoid space containing CSF extends slightly further caudally from the termination of the spinal cord into the lumbar cistern contained within the dural sac. In large dogs, the dural sac ends around the level of L7-S1, whereas in cats and small dogs it often extends as far caudally as the first sacral segment. Why is this information relevant? The likelihood of inadvertently performing a “wet tap” (puncturing the dural sac and allowing CSF to enter the needle) or an accidental intrathecal injection when performing a sacrococcygeal epidural significantly less than when compared to the approach to the lumbosacral space.
Indications
When local anesthetics are delivered into the epidural space, the goal is to block the associated spinal nerve roots. The location of nerve roots affected dictates the regions of the body that lose sensory and motor blockade for the duration of the epidural. As discussed above, the location of and typical medication doses for the sacrococcygeal or intercoccygeal epidural tend to yield a blockade limited to the perineal region. While urethral relaxation or temporary loss of anal tone are often noted, there should be no loss of pelvic limb motor function. Procedures in which a patient may benefit from a sacrococcygeal epidural include: catheterization for patients with urethral obstruction, tail amputation, deobstipation, anal sacculectomy, perineal urethrostomy and any other surgery of the perineal region. Lidocaine is typically used for procedures benefitting from rapid onset and duration (unblocking procedures, deobstipation) while bupivacaine is used for procedures that benefit from a longer duration of analgesia, but can permit a slower onset due to time for surgical preparation. The use of single-dose preservative-free local anesthetics is always ideal for sacrococcygeal epidurals, although 2% lidocaine with preservative can be used as long as the stopper is wiped with alcohol prior to puncture.
Materials
● Clippers and skin preparation solution
● Sterile gloves (ideally, but at minimum, exam gloves and careful consideration of contamination should be used)
● 0.1 ml/kg 2% lidocaine or 0.5% bupivacaine (up to 0.2 ml/kg has been reported for sacrococcygeal blocks, but the author typically finds that 0.1 ml/kg is sufficient)
● 25 or 22 GA hypodermic needle for cats or small dogs, 22 GA 1.5 in. spinal needle for medium-large breed dogs; very rarely a 20 GA 2.5 in. spinal needle is used for very large or obese dogs
● Syringe for volume of local anesthetic with separate needle for drawing up medications
● +/- sterile aperture drape

Technique
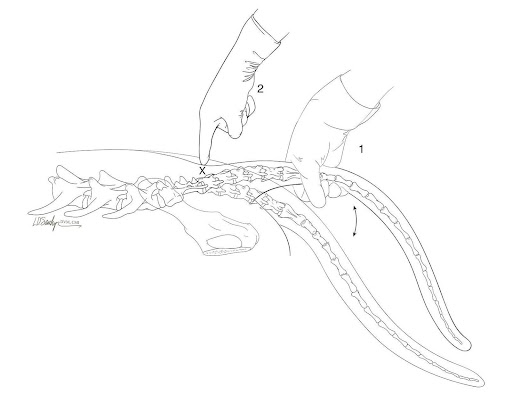
1. Position the sedated/anesthetized patient in sternal recumbency. Move the tail up and down in a pumping motion with one hand while using the other hand to palpate the first movable space at the caudal end of the sacrum. This will be the sacrococcygeal or intercoccygeal space (tip: it is often more cranial than you might expect by just looking at the patient!).
2. Clip a square area in the area you’ve palpated and prepare the skin aseptically for injection
3. Put on gloves and draw up the appropriate dose of medication in your syringe, ensuring that the needle used to draw up medications is switched out with a new needle for the block. (Note that if you are using a hypodermic needle for the epidural, the syringe can be attached directly to the needle. If you are using a spinal needle, you will proceed with the needle only and then attach the syringe for injection after you have removed the stylet from the needle. The stylet is typically removed after inserting a few mm., ensuring the needle will not be obstructed by skin and subcutaneous tissues.)
4. Place sterile aperture drape (if applicable)
5. Palpate the space again to confirm the location of injection. An assistant may pump the tail to confirm the point of sacral articulation.
6. Insert the needle through the skin on midline at an angle perpendicular to the skin. Proceed slowly; a small “pop” may be felt as the ligamentum flavum is traversed just dorsal to the epidural space.
7. If intense resistance from bone is encountered, withdraw the needle a few mm. and redirect cranially or caudally while remaining on midline. The author finds that tilting the needle-syringe more caudally, creating a flatter angle with the surface of the skin, tends to be most helpful.
8. If redirecting a few times does not yield success, remove the needle and syringe, re-palpate, and try again!
9. Once the needle enters the space, aspirate to ensure no blood or contamination, and slowly deliver the local anesthetic ensuring no resistance is felt during injection.

References & further reading
● Technique video (helpful overview; but note recommended needle size/doses differ from above):
https://www.youtube.com/watch?v=7PJvxQhoLwg
● https://www.aaha.org/resources/2020-aaha-anesthesia-and-monitoring-guidelines-for-dogs-and-cats/local-anesthetic-techniques/for-perineal-procedures/
● O’Hearn AK, Wright BD. Coccygeal epidural with local anesthetic for catheterization and pain management in the treatment of feline urethral obstruction. JVECC. 2011;21(1):50–21.
● Portela DA, Otero PE. Manual of Small Animal Regional Anesthesia. 5m Publishing; 2013.
● Campoy L, Read MR. Small Animal Regional Anesthesia and Analgesia. Wiley-Blackwell; 2019.

